Case of a 27 years old man with shortness of breath.
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent. This Elog reflects my patient-centred online learning portfolio.
This is the case of a 27 years old man, who is a daily wage labourer by profession and a resident of Iskilla.
CHIEF COMPLAINTS
The patient presented to the casualty with shortness of breath,4-5 episodes of loose stools from one day and 3-4 episodes of vomiting today.
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic one day ago. One day ago, he consumed at least 2 bottles of toddy and went to sleep. He had an episode of loose stools in his sleep. He had 4-5 episodes of loose stools and 3-4 episodes of vomiting in the night.He also had lower back pain. None of his family members experienced similar symptoms.
The following morning he felt hungry and consumed some milk. After consuming very little amount of milk he started to complain of shortness of breath and soon after became delirious and was unable to talk.
HISTORY OF PAST ILLNESS
He is not a known case of DM, HTN, TB or Asthma.
He has only visited a hospital once before, to take an injection to reduce his alcohol intake.
FAMILY HISTORY
No relevant family history.
PERSONAL HISTORY
The patient has been married for 5 years and has 2 daughters.
Diet- Mixed diet
Appetite- Normal
Sleep- Adequate
Bowel movement- 4-5 episodes of loose stools since one day.
Bladder movements- Normal
Addictions-
Alcohol-The patient is a regular consumer of alcohol for 15 years. He consumes alcohol or toddy every day.He started consuming alcohol 15 years ago because of peer pressure and work stress .Three years ago, he went to another hospital and took an injection in order to reduce his alcohol intake.He was in a facility for 23 days. His intake had reduced for a month and then increased again.
Tobacco- The patient is a regular consumer of tobacco . He chews at least one packet a day.
Smoking - No
VITALS(on admission)
Pulse rate- 120bpm
Respiratory rate- 40 /min
BP- 190/90 mmHg
SpO2- 60%
GRBS- 216 mg/dL
INVESTIGATIONS
ECG
13/2/22 (9:24 am)
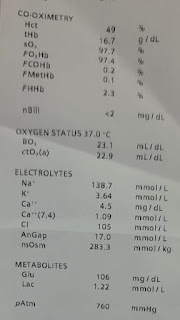
ABG
1.Day 1 - 12:35 pm
Day 1 -6:27 pm
RFT
Urea-21
Creatinine-0.8
Uric acid- 4
Calcium- 9.6
Phosporus- 6.2
Sodium- 144
Potassium- 4
Chloride- 100
LFT
TB-1.44
DB-0.65
AST- 40
ALT- 15
ALP- 169
TP-7.3
A/G-1.36
SERUM OSMOLALITY- 302.4
RBS- 125 mg /dl
HEMOGRAM
HB-17.9
TLC-4000
Neutrophils-85
Lymphocytes- 10
Eosinophils-1
Monocytes-4
Basophils -0
PCV- 53.4
MCV-90.1
MCH-30.2
MCHC-33.5
RBC-5.93
PT-2.06
RDW-CV-12.8
RDW-SD-42.5
Normocytic, Normochromic
DAY 2
Spot urine protein- 39
Spot urine creatinine- 123
APTT- 31 secs
PT- 15 secs
Complete urine examination-
Albumin- 3+
Sugars- 2+
RBS crystal casts- Nil
CHEST XRAY
PROVISIONAL DIAGNOSIS-
Type I respiratory failure
Secondary to aspiration pneumonia.
TREATMENT -
Head end elevation
RT feed - 100l free water 2nd Hourly, 50 ml milk 4th hourly
IV-20 NS at 75ml/Hour
INJ PIPTAZ 4.5gm IV-Stat
INJ PANTOP 40 mg IV OD
INJ ZOFER 4mg IV YID
Nebulations with mucomist 4th hourly
ABG -4th hourly
ECG - every 4 hours
INJ-Thiamine
DAY 2
VITALS
BP- 180/100 mmHg
PR-110bpm
RR-22 cycles per minute
FIO2-35 per cent
The patient showed spontaneous eye movements
The patient had spontaneous breathing plus mechanical ventilation.
Sedation was removed









Comments
Post a Comment