Case of a 51 years old man with loss of sensation in the left foot.
This is an online e log book to discuss our patient's de-identified health data shared after taking his/her/guardians' signed informed consent. This Elog reflects my patient-centred online learning portfolio.
This is the case of a 51 years old man, who is a farmer by occupation and a resident of West Bengal.
CHIEF COMPLAINT
The patient has a chief complaint of
- swelling of the left foot from 3 years.
- loss of all sensations in the left foot from 3 years.
- ulcer in the sole of the left foot from 11 months.
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 25 years ago, 25 years ago, while playing football the patient's left foot accidentally went into a ditch. This resulted in swelling of the left foot around the ankle joint, which was associated with continuous pain localised to the area below the ankle and not associated with any change in the colour of the overlying skin or fever. The pain aggravated on walking and was relieved on taking medication. Following this, he went to a doctor the next day, who prescribed him some medication. The patient took the medication for a week, and the swelling and pain subsided after a week.
3 years ago, during his morning walk, the patient's left foot accidentally went into a ditch. This led to the twisting of his ankle. Following this, the patient noticed swelling in the left foot. The swelling was predominantly towards the lateral side of the dorsum of the left foot and initially was associated with pain but, not associated with any change in the colour of the overlying skin and local rise of temperature.
Following, the onset of swelling and pain, the patient went to a doctor. An X-ray of the left foot was done, which revealed a crack near the base of the 5th metatarsal of the left foot. He was advised to undergo surgery, but he didn't and continued to take medicines for 9 months. The patient could walk with a limp, but his swelling did not subside.
After a week, the patient started experiencing tingling in his little toe of the left foot, which progressed medially. Followed by reduced sensations in the foot till the level of the ankle joint which progressed gradually. Now the patient is unable to perceive any sensations in the foot. The patient was also unable to dorsiflex his foot and described that his great toe kept dropping towards the floor, even when he tried to flex it. The patient complains that he was unable to wear his slippers and that the slippers would slip ahead and come off his foot. The swelling has caused him difficulty in walking and is hindering his daily work.
11 months ago, in November, the patient developed an ulcer in the medial aspect of the plantar region of his left foot which the patient initially did not notice as it was not associated with pain, bleeding, fever or changes in the surrounding skin. The patient complained of occasional watery discharge. Initially, the ulcer was small , when the patient went to the doctor. The doctor prescribed him an ointment for the ulcer, which did not give him any relief and eventually the ulcer progressed to being about 2-3 cms deep. On going to the doctor again after some weeks, he was prescribed some medications in addition to the ointment, which gave him some relief and the size of the ulcer reduced.The ulcer is still present.
HISTORY OF PAST ILLNESS
Not a known case
of DM, hypertension, asthma, TB, Thyroid condition, CVD, or Epilepsy.
FAMILY HISTORY
Father - known case of HTN
Mother- breathing difficulties
PERSONAL HISTORY
DIET- Mixed diet
APPETITE- Normal
SLEEP- Adequate
BOWEL
AND BLADDER MOVEMENTS - Normal
ADDICTIONS- Chews tobacco from 15 years . 10g in three days.
ALCOHOL- no
SMOKING-no
ALLERGIES- no
OCCUPATION HISTORY
The patient is a farmer who grows rice and jute . He has a history of standing for a long time in water and working .
DRUG HISTORY
PRESENT INVESTIGATIONS
24/9/2022
10/9/2022
PREVIOUS INVESTIGATIONS
3/1/2019
20/2/2019
29/10/2019
11/2/2020
16/9/21
GENERAL EXAMINATION
The patient is conscious, coherent and cooperative.
He is well built and well nourished.
Pallor- Absent
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Koilonychia- Absent
Pedal oedema- Absent
SYSTEMIC EXAMINATION
CNS
Patient is conscious and coherent.
Speech is normal.
Cranial nerves function - normal
Rt Lt
Reflexes- B Present Present
T Present Present
S Present Present
K Present Present
A Present Present
Left lower limb - Sensations absent
Dorsiflexion - negative
Plantar flexion- positive
CVS
S1 , S2 heard
No thrills
No murmurs
RESPIRATORY
Normal vesicular breath sounds heard
No wheeze or crepitations
Central position of the trachea
ABDOMEN
Obese abdomen
No tenderness
No hepatosplenomegaly
PROVISIONAL DIAGNOSIS
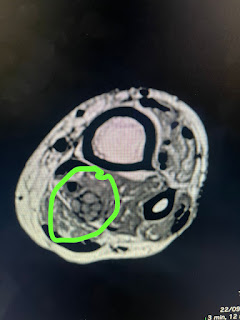
[12/09/22, 6:56:35 PM] Dr. Rakesh Biswas Sir General Med: @919398587059 Share his case case report [12/09/22, 6:56:56 PM] Bharat Sir GM: https://rishikakolotimedlog.blogspot.com/2022/09/51-year-old-male-with-swelling-and-loss.html?m=1 [12/09/22, 7:00:03 PM] Dr. Rakesh Biswas Sir General Med: Well done 👏👏 Please upload today's twist in the case where the neural ultrasound is suggesting a neural sheath tumor. Also in your description you may need to change thumb to great toe [12/09/22, 7:01:03 PM] Dr. Rakesh Biswas Sir General Med: @919398587059 Please share the ultrasound video images https://113riyagupta.blogspot.com/2022/09/case-of-51-years-old-man-with-loss-of.html?m=1 [12/09/22, 7:38:42 PM] Dr. Rakesh Biswas Sir General Med: Also when were his fractures and what is our Orthopedic comment on his fractures visible on the X-rays here ? [12/09/22, 7:45:11 PM] Riya Gupta: Yes sir [13/09/22, 2:45:57 PM] Dr. Rakesh Biswas Sir General Med: @919493340818 Please share the Dermat notes on their possibility of mycetoma [13/09/22, 3:05:15 PM] Charan Sir GM: image omitted [13/09/22, 3:05:28 PM] Charan Sir GM: image omitted [13/09/22, 3:06:02 PM] Charan Sir GM: image omitted [13/09/22, 5:03:36 PM] Dr. Rakesh Biswas Sir General Med: 👆Did you upload the same report in your case report yesterday? [13/09/22, 5:54:06 PM] Riya Gupta: Yes sir [14/09/22, 7:16:26 AM] Dr. Rakesh Biswas Sir General Med: @918522964349 check out the neurodegenerative changes on ultrasound of his nerves [14/09/22, 7:18:27 AM] Dr. Rakesh Biswas Sir General Med: This is a landmark case report that is currently going in the direction of infective neurodegeneration @918522964349 @8801733506870 Will be looking forward to your review of literature around this term. [14/09/22, 7:18:38 AM] Dr. Rakesh Biswas Sir General Med: [14/09/22, 8:12:11 AM] Dr. Rakesh Biswas Sir General Med: Please share his equine gait video and upload it to his case report [14/09/22, 8:18:11 AM] Dr.Charan: https://jnnp.bmj.com/content/76/suppl_2/ii23 This is one article on NCS with beautiful discription sir. Almost read 75% mostly will complete in 30 min sir [14/09/22, 8:24:32 AM] Dr. Rakesh Biswas Sir General Med: 👍Will be looking forward to your sharing the relevant portions with particular focus on this patient. Also please manage the morning and afternoon sessions and share the YouTubed video links in the academic session link [14/09/22, 9:51:12 AM] Riya Gupta: Uploaded sir [14/09/22, 9:56:10 AM] Dr. Rakesh Biswas Sir General Med: Good. In the diagnosis you need to mention the involved nerve and the fact that it is a mono neuropathy [14/09/22, 9:58:57 AM] Dr. Rakesh Biswas Sir General Med: Check out the video of another mononeuropathy published by our elective students long back here 👇 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4785487/ [14/09/22, 10:24:47 AM] Rishika Koloti: Done sir [14/09/22, 10:35:05 AM] Dr. Rakesh Biswas Sir General Med: Are you sure it's common peroneal and not distal to that? The patient's clinical signs suggest he has got good power in calf muscles as well as sensation over it's dermatome? Which nerve supplies there? And which nerve supplies till the dorsum which is the most affected? [14/09/22, 11:41:24 AM] Riya Gupta: Sir the calf muscles are being supplied by the tibial nerve and the patient is able to plantarflex . The major part of the sensory supply of dorsum is supplied by the superficial peroneal nerve ( branch of common peroneal) . The sensory supply of the foot also involve other nerves like Sural nerve , Saphenous nerve and distal branches of the Tibial nerve in the plantar aspect .He is not able to dorsiflex due to the involvement of the deep peroneal nerves . [14/09/22, 11:42:02 AM] Riya Gupta: Sir since there is no sensation in the entirety of the foot , could this be a polyneuropathy ? [14/09/22, 11:42:10 AM] b Rishika Koloti: https://www.ncbi.nlm.nih.gov/mesh/68020427 Peroneal Neuropathies Disease involving the common PERONEAL NERVE or its branches, the deep and superficial peroneal nerves. Lesions of the deep peroneal nerve are associated with PARALYSIS of dorsiflexion of the ankle and toes and loss of sensation from the web space between the first and second toe. Lesions of the superficial peroneal nerve result in weakness or paralysis of the peroneal muscles (which evert the foot) and loss of sensation over the dorsal and lateral surface of the leg. [14/09/22, 11:42:11 AM] Rishika Koloti: Tibial Neuropathy Clinical features include PARALYSIS of plantar flexion, ankle inversion and toe flexion as well as loss of sensation over the sole of the foot. (From Joynt, Clinical Neurology, 1995, Ch51, p32) Year introduced: 2000 https://www.ncbi.nlm.nih.gov/mesh/68020429 [14/09/22, 11:47:26 AM] Rishika Koloti: Suggestive of deep peroneal nerve involvement - -Absence of dorsiflexion -loss of sensation in first web space Suggestive of tibial involvement- Loss of sensation over sole of foot [14/09/22, 8:53:34 PM] Dr. Rakesh Biswas Sir General Med: Thanks. Well analyzed both of you 👏 So do we have the findings in this particular patient that we have now reviewed in terms of general knowledge? We know our patient has findings of PARALYSIS of dorsiflexion in his ankle and toes and loss of sensation from the web space between the first and second toe suggestive of deep peroneal? But have we checked for paralysis of the peroneal muscles (which evert the foot) and loss of sensation over the dorsal and lateral surface of the leg that would also suggest superficial peroneal nerve? I guess his tibial nerve is intact? So now we come to the question of nomenclature. When would we call it mononeuropathy? What if the entire sciatic nerve is involved? Will that still be a mononeuropathy or polyneuropathy? [15/09/22, 4:16:01 PM] Rishika Koloti : Goodevening sir , we went to pathology , his results were not there as yet [18/09/22, 9:27:31 AM] Dr. Rakesh Biswas Sir General Med: @Please update the fact that we have sent his biopsy from ear lobules and skin ulcer. Also upload the image of the histopathology findings that are going to be presented tomorrow in the clinico diagnostic meet by @ along with the Dermatology and pathology PGs. [18/09/22, 12:16:53 PM] Rishika Koloti: Yes sir [18/09/22, 6:54:54 PM] Dr. Rakesh Biswas Sir General Med: Please add all the current student volunteers to this and the other two current neurodegenerative groups (one still online and the other gone to MNJ with leukemia) to build the conversational learning outcomes that will demonstrably drive these patients disease outcomes. [18/09/22, 6:59:45 PM] Dr. Rakesh Biswas Sir General Med: Here for this patient, let me begin by asking this basic STEM question : What is wallerian degeneration and how is it related to infective or any other inflammatory injury including trauma? How are neurodegenerative disorders different in terms of their neuronal degeneration? [18/09/22, 7:02:07 PM] Dr. Rakesh Biswas Sir General Med: This patient is also being presented tomorrow and his link is also accessible here 👇 https://medicinedepartment.blogspot.com/2022/09/two-cases-for-monday-clinico-diagnostic.html?m=1 [18/09/22, 7:02:24 PM] Sanjana: Ok sir [18/09/22, 7:03:34 PM] Dr. Rakesh Biswas Sir General Med: 👆Anyone here can start the ball rolling here on the answers to these questions. Feel free to use Google optimally [19/09/22, 5:48:43 PM] Dr Charan: Tomorrow planned for sural nerve biopsy in OT sir. Surgeons ordered few investigations and OT drug list. Under local anesthesia. Please look into this and send coagulation profile and necessary investigations and make sure patient is ready with OT drugs. Thank you [19/09/22, 7:35:17 PM] Sanjana: https://jneuroinflammation.biomedcentral.com/articles/10.1186/1742-2094-8-109 The characteristics of an efficient innate-immune response are rapid onset and conclusion, and the orchestrated interplay between Schwann cells, fibroblasts, macrophages, endothelial cells, and molecules they produce. Wallerian degeneration serves as a prelude for successful repair when these requirements are met. In contrast, functional recovery is poor when injury fails to produce the efficient innate-immune response of Wallerian degeneration. [19/09/22, 9:14:19 PM] Dr. Rakesh Biswas Sir General Med: [9/19, 12:24 PM] Dr. Navaneetha : Sir only slit skin smear done and sent to microbiology sir.... Not biopsy.... Only microbiology dept. Involved.... Not pathology [9/19, 1:18 PM] Rakesh Biswas: No biopsy taken from the planter area where he had a perforating ulcer? [9/19, 1:34 PM] Dr. Navaneetha: No sir [9/19, 1:34 PM]Dr. Navaneetha: We did culture sensitive from ulcer... [9/19, 7:43 PM]Dr. Rakesh Biswas: The slit skin came negative from the department of Microbiology. Tomorrow we are getting a sural nerve biopsy done by Prof Krishnamurti to rule out a pure neuritic leprosy. Would be grateful for any suggestions from your end [9/19, 7:45 PM]Dr. Navaneetha : Yes sir nerve biopsy is best option.... Before that high resolution USG of nerve will tell us is their any inflammation of the nerve [9/19, 9:12 PM]Dr. Rakesh Biswas: That was already done a week ago from KHL. Check out his case report link in the link shared above [19/09/22, 9:16:19 PM]Dr. Charan : image omitted [19/09/22, 9:16:44 PM]Dr. Charan : image omitted [19/09/22, 9:17:11 PM] Charan Sir GM: please update this reports in blog. [19/09/22, 9:18:06 PM] Riya Gupta: Updated sir [19/09/22, 9:18:17 PM]Dr. Charan : Thank you [19/09/22, 10:26:27 PM] Dr. Rakesh Biswas Sir General Med: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8354402/ [19/09/22, 10:26:28 PM] Dr. Rakesh Biswas Sir General Med: image omitted [19/09/22, 10:26:28 PM] Dr. Rakesh Biswas Sir General Med: image omitted [19/09/22, 10:29:06 PM] Dr. Rakesh Biswas Sir General Med: That's a very interesting take on Wallerian degeneration! Neurodegenerative disorders on the contrary are disorders that tend to deteriorate. Tell us more about Wallerian degeneration and it's differences with usual neurodegenerative disorders [19/09/22, 10:58:44 PM] Dr Charan: “Neurodegeneration” is a commonly used word whose meaning is believed to be universally understood. Yet finding a precise definition for neurodegeneration is much more arduous than one might imagine. Often, neurodegeneration is only casually mentioned and scarcely discussed in major medical textbooks and is even incompletely defined in the most comprehensive dictionaries. Etymologically, the word is composed of the prefix “neuro-,” which designates nerve cells (i.e., neurons), and “degeneration,” which refers to, in the case of tissues or organs, a process of losing structure or function. Thus, in the strict sense of the word, neurodegeneration corresponds to any pathological condition primarily affecting neurons. In practice, neurodegenerative diseases represent a large group of neurological disorders with heterogeneous clinical and pathological expressions affecting specific subsets of neurons in specific functional anatomic systems; they arise for unknown reasons and progress in a relentless manner https://www.ncbi.nlm.nih.gov/pmc/articles/PMC151843/ [19/09/22, 11:04:02 PM]Dr. Charan: Neuronal and axonal degeneration, as well as inflammation and demyelination, are integral components of the pathology of multiple sclerosis (MS). Neurodegeneration is seen in the earliest stages and throughout the course of the disease and contributes to irreversible physical and cognitive disability. Mitochondrial malfunction and energy failure, loss of trophic support by myelin, ion channel dysfunction, oxidative stress, and excitotoxicity have been identified as possible contributors to neurodegeneration https://www.sciencedirect.com/topics/medicine-and-dentistry/nerve-cell-degeneration [19/09/22, 11:06:18 PM] Dr Charan: Going by above two reviews it appears as Neuronal degeneration ( either axon or cell body ) is the basic and early contributor for neurodegeneration ( group of diseases with similar patterns of involvement)..? [20/09/22, 7:38:33 AM] Dr. Rakesh Biswas Sir General Med: Share the above in the AJND PaJR group [25/09/22, 4:18:08 AM] Sanjana: image omitted [25/09/22, 9:05:32 AM] Dr. Rakesh Biswas Sir General Med: Thanks for sharing this. Can you share the related mri findings from our radspa [25/09/22, 9:06:26 AM] Sanjana: Sir I've been told that radspa is not working [25/09/22, 9:08:32 AM] Dr. Rakesh Biswas Sir General Med: Please ask one of the duty interns to check and revert asap [25/09/22, 10:00:30 AM] Dr. Rakesh Biswas Sir General Med: Excellent and team. Please go through google images of normal leg mri and learn the normal anatomy visible and then identify the pathology seen in your patient followed by labelling them in the images you shared. [25/09/22, 10:02:56 AM] Rishika Koloti : Yes sir [25/09/22, 1:32:32 PM] : image omitted [25/09/22, 1:33:28 PM] : image omitted [25/09/22, 1:33:47 PM] : image omitted [25/09/22, 1:39:01 PM] Dr. Rakesh Biswas Sir General Med: Where does the common peroneal nerve begin and is this cross sectional view in that region? [25/09/22, 1:46:01 PM] Dr. Rakesh Biswas Sir General Med: Can you share the examination findings reflecting the current physiological functioning of his left common peroneal and tibial nerve in this patient? Again Can take this discussion to the PaJR group or AJND group so as not to spam the patient's advocates here [25/09/22, 2:31:57 PM]Rishika Koloti: Suggestive of tibial nerve involvement- 1. Loss of sensation over sole of foot Suggestive of deep peroneal nerve involvement 1. Absence of dorsifelxion of ankle 2. Loss of sensation from first web space between first and second toe Suggestive of superficial peroneal nerve involvement 1. Inability to evert the foot https://www.ncbi.nlm.nih.gov/mesh/68020427 https://www.ncbi.nlm.nih.gov/mesh/68020429 [25/09/22, 2:38:52 PM]Rishika Koloti : And loss of sensation over dorsum of foot for superficial peroneal nerve [25/09/22, 2:50:53 PM] Dr. Rakesh Biswas Sir General Med: So involvement of tibial is only sensory while the involvement of common peroneal is motor sensory? [25/09/22, 3:00:00 PM] Riya Gupta: Sir the ankle reflex is present and he is able to plantar flex , hence the motor component of the tibial nerve supplying the calf muscles is not involved . [25/09/22, 3:06:00 PM] Dr. Rakesh Biswas Sir General Med: all the important conversations around this patient above needs to be archived in the discussion section of your case report and all these need to be archived in your AJND paper [25/09/22, 3:06:27 PM] Sanjana: Yes sir noted [25/09/22, 3:06:30 PM] Rishika Koloti : Yes sir [26/09/22, 10:07:33 PM] Dr. Rakesh Biswas Sir General Med: Please check in class tomorrow if the patient lost just his pain sensation in his left ankle and planter dermatomes or did he also lose his perception of fine touch. If there is dissociative anesthesia (preserved fine touch but absent pain) then it would be pure small fibre neuropathy that can explain his preserved reflexes (reflexes are carried by the large fibers) Check out the literature to see where this has been reported and if none available let's report this text book fact as a BMJ Case report particularly for this patient [26/09/22, 10:15:17 PM]Rishika Koloti: Sir, when we had examined, propioception was present ,*fine touch and pain was absent* . We shall talk to the patient again tomorrow to confirm . [26/09/22, 10:15:37 PM] Rishika Koloti: Yes sir will look it up [26/09/22, 10:19:30 PM]Dr. Deepika Gm: Hip - Flexion, Extension, abduction, adduction, medial and lateral rotation Rt and left - normal Knee- Flexion Extension normal Ankle - Dorsiflexion absent on left foot Plantarflexion present Inversion present Eversion absent left foot Loss of toe Extension Reflexes : Well preserved Knee jerk ++ Ankle jerk ++ Plantar flexor- rt. mute - lt Sensory exmtn: Spinothalamic: Crudetouch pain temperature present bilaterally upto ankle Lost below left ankle Posterior column: Fine touch , vibration lost below ankle left side Vibration decreased on rt lowerlimb at level of ankle Proprioception rt 9/10. Left 5/10 Cortical: Graphestesia + rt side - lt side @ ankle Thickened nerves + At Knee joint palpable common peroneal nerve Foot drop present [26/09/22, 10:34:49 PM] Dr. Rakesh Biswas Sir General Med: Mention the power grade where it is other than normal In sensory mention the dermatomes , proprioception mention the joints, You have classified sensory as per spinal cord although it's a peripheral neuropathy Thickened common peroneal? Where? [26/09/22, 10:46:31 PM]Dr. Deepika : Prorioception I did at the great toe sir Dermatomal level i couldn't clearly delineate sir bcoz part of dermatome sensations were present wherein the other part were absent I.e, above ankle few sensations were preserved and below were lost in same dermatome Thickened peroneal nerve @level of knee joint lateral aspect of knee [26/09/22, 10:48:26 PM] Dr. Rakesh Biswas Sir General Med: Both sides? Palpable? [26/09/22, 10:49:26 PM] Dr. Rakesh Biswas Sir General Med: For a peripheral neuropathy the spinothalamic is mentioned as small fibre while posterior column as large fibre [26/09/22, 10:50:42 PM] Dr. Rakesh Biswas Sir General Med: Bring him to class again tomorrow [27/09/22, 1:17:06 PM]Dr. Bharat : video omitted [27/09/22, 1:58:37 PM]Dr. Deepika : Unilateral sir [27/09/22, 2:02:24 PM]Dr. Bharat: video omitted [30/09/22, 9:38:57 AM] Dr. Rakesh Biswas Sir General Med: Share his discharge summary in the case report. Also add the nerve mri images https://113riyagupta.blogspot.com/2022/09/case-of-51-years-old-man-with-loss-of.html?m=1 [30/09/22, 9:39:35 AM] Dr. Rakesh Biswas Sir General Med: Also add Tab Amitryptiline 25 mg one hour before dinner everyday [08/10/22, 9:53:36 AM]: image omitted [08/10/22, 9:53:37 AM]: image omitted [08/10/22, 9:53:37 AM] : image omitted [08/10/22, 9:53:37 AM] : image omitted [08/10/22, 9:53:38 AM] : image omitted [08/10/22, 9:55:11 AM] : স্যার পা ফুলাটা এখনো কমেনি [08/10/22, 9:57:11 AM] Dr. Rakesh Biswas Sir General Med: Eta theke poonj beruchhena to? [08/10/22, 10:14:04 AM] patient attender: Na sir [25/12/22, 2:26:47 PM]: image omitted








































Comments
Post a Comment